This syringe contains a radioactive form of glucose known as FDG. The doctor will soon inject its contents into her patient’s arm, whom she’s testing for cancer using a PET scanner. The FDG will quickly circulate through his body. If he has a tumor, cancer cells within it will take up a significant portion of the FDG, which will act as a beacon for the scanner. PET tracers such as FDG are among the most remarkable tools in medical diagnostics, and their life begins in a particle accelerator, just hours earlier.
The particle accelerator in question is called a cyclotron, and it’s often housed in a bunker within hospitals. It uses electromagnetic fields to propel charged particles like protons faster and faster along a spiraling path. When the protons reach their maximum speed, they shoot out onto a target that contains a few milliliters of a type of water with a heavy form of oxygen called oxygen-18. When a proton slams into one of these heavier oxygen atoms, it kicks out another subatomic particle called a neutron. This impact turns oxygen-18 into fluorine-18, a radioactive isotope that can be detected on a PET scan. In a little under two hours, about half the fluorine will be gone due to radioactive decay, so the clock is ticking to get the scan done.
So how can fluorine-18 be used to detect diseases? Radiochemists at the hospital can use a series of chemical reactions to attach the radioactive fluorine to different molecules, creating radiotracers. The identity of the tracer depends on what doctors want to observe. FDG is a common one because the rate at which cells consume glucose can signal the presence of cancer; the location of an infection; or the slowing brain function of dementia.
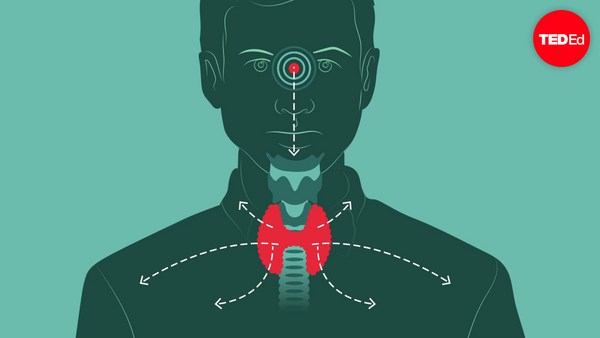
The FDG is now ready for the patient’s scan. When a radiolabeled tracer enters the body, it travels through the circulatory system and gets taken up by its target— whether that's a protein in the brain, cancer cells, or otherwise. Within a few minutes, a significant amount of the tracer has found its way to the target area and the rest has cleared from circulation. Now the doctors can see their target using a PET, or positron emission tomography, scanner.
The radiation that the tracer emits is what makes this possible. The isotopes used in PET decay by positron emission. Positrons are essentially electrons with positive charge. When emitted, a positron collides with an electron from another molecule in its surroundings. This causes a tiny nuclear reaction in which the mass of the two particles is converted into two high-energy photons, similar to X-rays, that shoot out in opposite directions. These photons will then impact an array of paired radiation detectors in the scanner walls. The software in the scanner uses those detectors to estimate where inside the body the collision occurred and create a 3D map of the tracer’s distribution. PET scans can detect the spread of cancer before it can be spotted with other types of imaging. They’re also revolutionizing the diagnosis of Alzheimer’s disease by allowing doctors to see amyloid, the telltale protein buildup that otherwise couldn’t be confirmed without an autopsy. Meanwhile, researchers are actively working to develop new tracers and expand the possibilities of what PET scans can be used for.
But with all this talk of radiation and nuclear reactions inside the body, are these scans safe? Even though no amount of ionizing radiation is completely safe, the amount of radiation the body receives during a PET scan is actually quite low. One scan is comparable to what you’re exposed to over two or three years from natural radioactive sources, like radon gas; or the amount a pilot would rack up from cosmic radiation after 20 to 30 transatlantic flights. Most patients feel that those risks are acceptable for the chance to diagnose and treat their illnesses.