At any given moment, trillions of cells are traveling through your blood vessels, sometimes circling the body in just one minute. Each of these cells has its origins deep in your bones. Bones might seem rock-solid, but they’re actually quite porous inside. Large and small blood vessels enter through these holes. And inside most of the large bones of your skeleton is a hollow core filled with soft bone marrow. Marrow contains fat and other supportive tissue, but its most essential elements are blood stem cells. These stem cells are constantly dividing. They can differentiate into red blood cells, white blood cells, and platelets, and send about hundreds of billions of new blood cells into circulation every day. These new cells enter the bloodstream through holes in small capillaries in the marrow. Through the capillaries, they reach larger blood vessels and exit the bone.
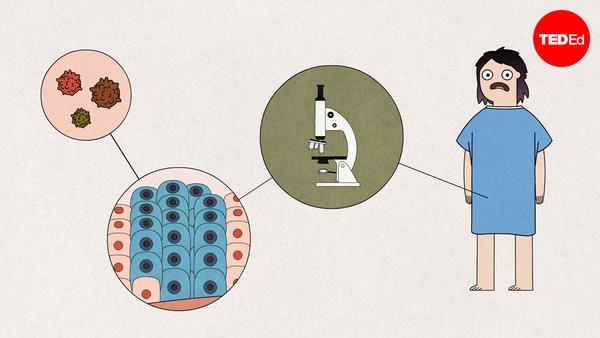
If there’s a problem with your blood, there’s a good chance it can be traced back to the bone marrow. Blood cancers often begin with genetic mutations in the stem cells. The stem cells themselves are not cancerous, but these mutations can interfere with the process of differentiation and result in malignant blood cells. So for patients with advanced blood cancers like leukemia and lymphoma, the best chance for a cure is often an allogeneic bone marrow transplant, which replaces the patient’s bone marrow with a donor’s.
Here’s how it works. First, blood stem cells are extracted from the donor. Most commonly, blood stem cells are filtered out of the donor’s bloodstream by circulating the blood through a machine that separates it into different components. In other cases, the marrow is extracted directly from a bone in the hip, the iliac crest, with a needle.
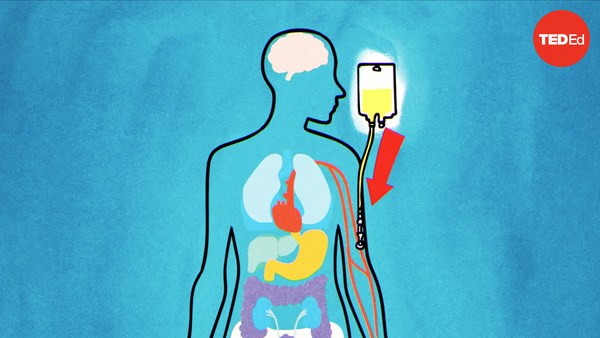
Meanwhile, the recipient prepares for the transplant. High doses of chemotherapy or radiation kill the patient’s existing marrow, destroying both malignant cells and blood stem cells. This also weakens the immune system, making it less likely to attack the transplanted cells. Then the donor cells are infused into the patient’s body through a central line. They initially circulate in the recipient’s peripheral bloodstream, but molecules on the stem cells, called chemokines, act as homing devices and quickly traffic them back to the marrow. Over the course of a few weeks, they begin to multiply and start producing new, healthy blood cells. Just a small population of blood stem cells can regenerate a whole body’s worth of healthy marrow.
A bone marrow transplant can also lead to something called graft-versus-tumor activity, when new immune cells generated by the donated marrow can wipe out cancer cells the recipient’s original immune system couldn’t. This phenomenon can help eradicate stubborn blood cancers. But bone marrow transplants also come with risks, including graft-versus-host disease. It happens when the immune system generated by the donor cells attacks the patient’s organs. This life-threatening condition occurs in about 30–50% of patients who receive donor cells from anyone other than an identical twin, particularly when the stem cells are collected from the blood as opposed to the bone marrow.
Patients may take immunosuppressant medications or certain immune cells may be removed from the donated sample in order to reduce the risk of graft-versus-host disease. But even if a patient avoids graft-versus-host disease, their immune system may reject the donor cells. So it’s crucial to find the best match possible in the first place.
Key regions of the genetic code determine how the immune system identifies foreign cells. If these regions are similar in the donor and the recipient, the recipient’s immune system is more likely to accept the donor cells. Because these genes are inherited, the best matches are often siblings. But many patients who need a bone marrow transplant don’t have a matched family member. Those patients turn to donor registries of volunteers willing to offer their bone marrow.
All it takes to be on the registry is a cheek swab to test for a genetic match. And in many cases, the donation itself isn’t much more complicated than giving blood. It’s a way to save someone’s life with a resource that’s completely renewable.