During World War I, one of the horrors of trench warfare was a poisonous yellow cloud called mustard gas. For those unlucky enough to be exposed, it made the air impossible to breathe, burned their eyes, and caused huge blisters on exposed skin.
Scientists tried desperately to develop an antidote to this vicious weapon of war. In the process they discovered the gas was irrevocably damaging the bone marrow of affected soldiers— halting its ability to make blood cells. Despite these awful effects, it gave scientists an idea. Cancer cells share a characteristic with bone marrow: both replicate rapidly. So could one of the atrocities of war become a champion in the fight against cancer? Researchers in the 1930s investigated this idea by injecting compounds derived from mustard gas into the veins of cancer patients. It took time and trial and error to find treatments that did more good than harm, but by the end of World War II, they discovered what became known as the first chemotherapy drugs.
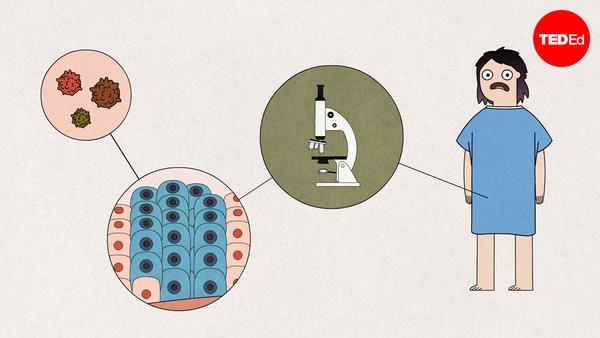
Today, there are more than 100. Chemotherapy drugs are delivered through pills and injections and use "cytotoxic agents," which means compounds that are toxic to living cells. Essentially, these medicines cause some level of harm to all cells in the body— even healthy ones. But they reserve their most powerful effects for rapidly-dividing cells, which is precisely the hallmark of cancer.
Take, for example, those first chemotherapy drugs, which are still used today and are called alkylating agents. They’re injected into the bloodstream, which delivers them to cells all over the body. Once inside, when the cell exposes its DNA in order to copy it, they damage the building blocks of DNA’s double helix structure, which can lead to cell death unless the damage is repaired. Because cancer cells multiply rapidly, they take in a high concentration of alkylating agents, and their DNA is frequently exposed and rarely repaired. So they die off more often than most other cells, which have time to fix damaged DNA and don’t accumulate the same concentrations of alkylating agents.
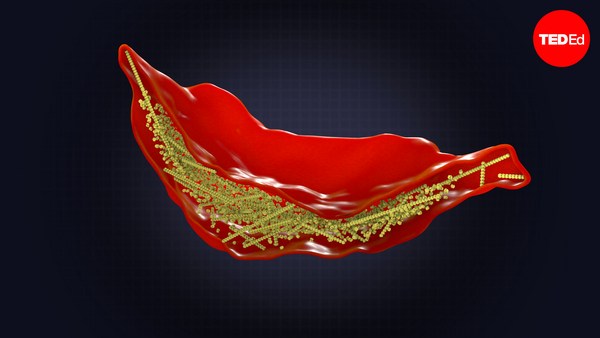
Another form of chemotherapy involves compounds called microtubule stabilizers. Cells have small tubes that assemble to help with cell division and DNA replication, then break back down. When microtubule stabilizers get inside a cell, they keep those tiny tubes from disassembling. That prevents the cell from completing its replication, leading to its death.
These are just two examples of the six classes of chemotherapy drugs we use to treat cancer today. But despite its huge benefits, chemotherapy has one big disadvantage: it affects other healthy cells in the body that naturally have to renew rapidly. Hair follicles, the cells of the mouth, the gastrointestinal lining, the reproductive system, and bone marrow are hit nearly as hard as cancer.
Similar to cancer cells, the rapid production of these normal cells means that they’re reaching for resources more frequently— and are therefore more exposed to the effects of chemo drugs. That leads to several common side effects of chemotherapy, including hair loss, fatigue, infertility, nausea, and vomiting. Doctors commonly prescribe options to help manage these side-effects, such as strong anti-nausea medications. For hair loss, devices called cold caps can help lower the temperature around the head and constrict blood vessels, limiting the amount of chemotherapy drugs that reach hair follicles. And once a course of chemo treatment is over, the healthy tissues that’ve been badly affected by the drug will recover and begin to renew as usual.
In 2018 alone, over 17 million people world-wide received a cancer diagnosis. But chemotherapy and other treatments have changed the outlook for so many. Just take the fact that up to 95% of individuals with testicular cancer survive it, thanks to advances in treatment. Even in people with acute myeloid leukemia— an aggressive blood cancer— chemotherapy puts an estimated 60% of patients under 60 into remission following their first phase of treatment.
Researchers are still developing more precise interventions that only target the intended cancer cells. That’ll help improve survival rates while leaving healthy tissues with reduced harm, making one of the best tools we have in the fight against cancer even better.