In 1881, doctor William Halsted rushed to help his sister Minnie, who was hemorrhaging after childbirth. He quickly inserted a needle into his arm, withdrew his own blood, and transferred it to her. After a few uncertain minutes, she began to recover.
Halsted didn’t know how lucky they’d gotten. His transfusion only worked because he and his sister happened to have the same blood type— something that isn’t guaranteed, even among close relatives.
Blood types hadn’t been discovered by Halsted’s time, though people had been experimenting with transfusions for centuries— mostly unsuccessfully. In 1667, a French physician named Jean-Baptiste Denis became the first to try the technique on a human. Denis transfused sheep’s blood into Antoine Mauroy, a man likely suffering from psychosis, in the hopes that it would reduce his symptoms. Afterward, Mauroy was in good spirits. But after a second transfusion, he developed a fever, severe pain in his lower back, intense burning in his arm, and he urinated a thick, black liquid.
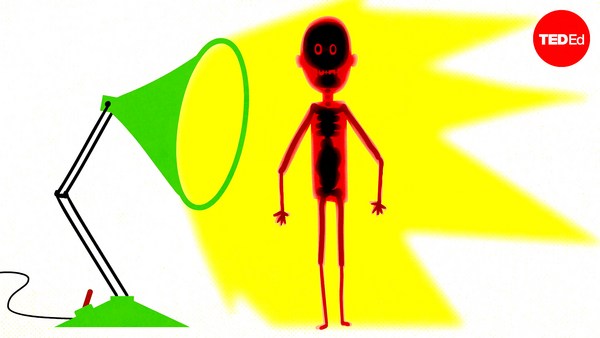
Though nobody knew it at the time, these were the signs of a dangerous immune response unfolding inside his body. This immune response starts with the production of proteins called antibodies, which distinguish the body’s own cells from intruders. They do so by recognizing the foreign proteins, or antigens, embedded in an intruder’s cell membrane. Antibodies latch onto the antigens, signaling other immune cells to attack and destroy the foreign cells.
The destroyed cells are flushed from the body in urine. In extreme cases, the massive break down of cells causes clots in the bloodstream that disrupt the flow of blood to vital organs, overload the kidneys, and cause organ failure. Fortunately, Denis’s patient survived the transfusion. But, after other cross-species transfusions proved fatal, the procedure was outlawed across Europe, falling out of favor for several centuries.
It wasn’t until 1901 that Austrian physician Karl Landsteiner discovered blood types, the crucial step in the success of human to human blood transfusions. He noticed that when different types were mixed together, they formed clots. This happens when antibodies latch on to cells with foreign antigens, causing blood cells to clump together. But if the donor cells are the same blood type as the recipient’s cells, the donor cells won’t be flagged for destruction, and won’t form clumps.
By 1907, doctors were mixing together small amounts of blood before transfusing it. If there were no clumps, the types were a match. This enabled them to save thousands of lives, laying the foundation for modern transfusions.
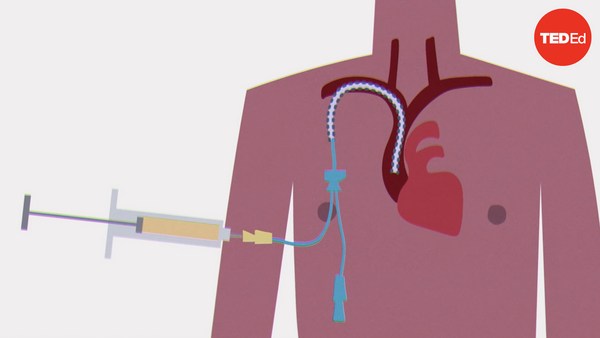
Up to this point, all transfusions had occurred in real time, directly between two individuals. That’s because blood begins to clot almost immediately after coming into contact with air— a defense mechanism to prevent excessive blood loss after injury.
In 1914, researchers discovered that the chemical sodium citrate stopped blood coagulating by removing the calcium necessary for clot formation. Citrated blood could be stored for later use— the first step in making large scale blood transfusions possible. In 1916, a pair of American scientists found an even more effective anticoagulant called heparin, which works by deactivating enzymes that enable clotting. We still use heparin today.
At the same time, American and British researchers developed portable machines that could transport donor blood onto the battlefields of World War I. Combined with the newly-discovered heparin, medics safely stored and preserved liters of blood, wheeling it directly onto the battlefield to transfuse wounded soldiers.
After the war, this crude portable box would become the inspiration for the modern-day blood bank, a fixture of hospitals around the world.