London, 1928: a group of mold spores surf a breeze through a lab. They drift onto a petri dish, and when they land, they germinate a medical revolution. This lab belongs to Alexander Fleming, a Scottish scientist investigating the properties of infectious bacteria. At this time, Fleming is away on vacation. When he returns, he finds a colony of mold growing on a petri dish he’d forgotten to place in his incubator. And around this colony of mold is a zone completely and unexpectedly clear of bacteria.
In studying this mysterious phenomenon, Fleming came to realize that the mold was secreting some kind of compound that was killing the bacteria. The mold was a species in the Penicillium genus, so Fleming dubbed the antibacterial compound “penicillin.”
What Fleming stumbled upon was a microbial defense system. The penicillium mold constantly produces penicillin in order to defend itself from threats, such as nearby bacterial colonies that might consume its resources. Penicillin destroys many types of bacteria by disrupting synthesis of their cell walls. These walls get their strength from a thick, protective mesh of sugars and amino acids, that are constantly being broken down and rebuilt. Penicillin binds to one of the compounds that weaves this mesh together and prevents the wall from being reconstructed at a critical phase. Meanwhile, penicillin stimulates the release of highly reactive molecules that cause additional damage. Eventually, the cell’s structure breaks down completely. This two-pronged attack is lethal to a wide range of bacteria, whether in petri-dishes, our bodies, or elsewhere. It’s not, however, harmful to our own cells, because those don’t have cell walls.
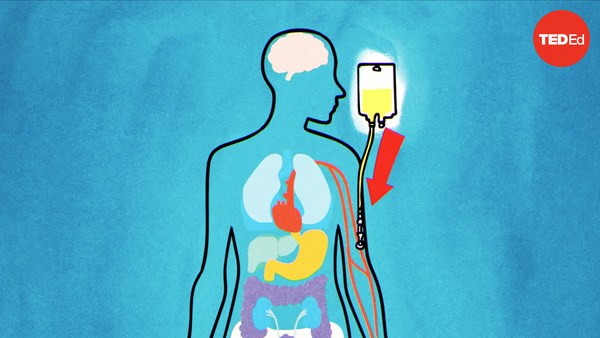
For a decade or so after Fleming’s discovery, penicillin remained a laboratory curiosity. But during World War II, researchers figured out how to isolate the active compound and grow the mold in larger quantities. They then went on to win the Nobel Prize for their work. Teams at Oxford and several American drug companies continued development, and within a few years it was commercially available. Penicillin and similar compounds quickly transformed the treatment of infections. For the time being, they remain some of the most important, life-saving antibiotics used in medicine.
However, the more we use any antibiotic, the more bacteria evolve resistance to it. In the case of penicillin, some bacteria produce compounds that can break down the key structure that interferes with cell wall synthesis. As antibiotic use has increased, more and more bacteria have evolved this defense, making these antibiotics ineffective against a growing number of bacterial infections. This means it’s essential that doctors not overprescribe the drug.
Meanwhile, 5 to 15% of patients in developed countries self-identify as allergic to penicillin, making it the most commonly reported drug allergy. However, the vast majority— over 90%— of people who think they’re allergic to penicillin actually are not. Why the misperception? Many patients acquire the allergy label as children, when a rash appears after they’re treated for an infection with penicillin or closely related drugs. The rash is often blamed on penicillin, while the more likely culprit is the original infection, or a reaction between the infection and the antibiotic. However, genuine penicillin allergies, where our immune systems mistake penicillin for an attacker, do occur rarely and can be very dangerous. So if you think you’re allergic but don’t know for sure, your best bet is to visit an allergist. They’ll complete an evaluation that’ll confirm whether or not you have the allergy.
Even if you do have a penicillin allergy, your immune cells that react to the drug may lose their ability to recognize it. In fact, about 80% of people who are allergic to penicillin outgrow their allergy within ten years. This is great news for people who currently identify as allergic to penicillin; the drug may one day save their lives, as it has done for so many others.