The first patient to ever be treated with an antibiotic was a policeman in Oxford. On his day off from work, he was scratched by a rose thorn while working in the garden. That small scratch became infected. Over the next few days, his head was swollen with abscesses, and in fact his eye was so infected that they had to take it out, and by February of 1941, this poor man was on the verge of dying. He was at Radcliffe Infirmary in Oxford, and fortunately for him, a small team of doctors led by a Dr. Howard Florey had managed to synthesize a very small amount of penicillin, a drug that had been discovered 12 years before by Alexander Fleming but had never actually been used to treat a human, and indeed no one even knew if the drug would work, if it was full of impurities that would kill the patient, but Florey and his team figured if they had to use it, they might as well use it on someone who was going to die anyway.
So they gave Albert Alexander, this Oxford policeman, the drug, and within 24 hours, he started getting better. His fever went down, his appetite came back. Second day, he was doing much better. They were starting to run out of penicillin, so what they would do was run with his urine across the road to re-synthesize the penicillin from his urine and give it back to him, and that worked. Day four, well on the way to recovery. This was a miracle. Day five, they ran out of penicillin, and the poor man died.
So that story didn't end that well, but fortunately for millions of other people, like this child who was treated again in the early 1940s, who was again dying of a sepsis, and within just six days, you can see, recovered thanks to this wonder drug, penicillin. Millions have lived, and global health has been transformed. Now, antibiotics have been used for patients like this, but they've also been used rather frivolously in some instances, for treating someone with just a cold or the flu, which they might not have responded to an antibiotic, and they've also been used in large quantities sub-therapeutically, which means in small concentrations, to make chicken and hogs grow faster. Just to save a few pennies on the price of meat, we've spent a lot of antibiotics on animals, not for treatment, not for sick animals, but primarily for growth promotion.
Now, what did that lead us to? Basically, the massive use of antibiotics around the world has imposed such large selection pressure on bacteria that resistance is now a problem, because we've now selected for just the resistant bacteria.
And I'm sure you've all read about this in the newspapers, you've seen this in every magazine that you come across, but I really want you to appreciate the significance of this problem. This is serious. The next slide I'm about to show you is of carbapenem resistance in acinetobacter. Acinetobacter is a nasty hospital bug, and carbapenem is pretty much the strongest class of antibiotics that we can throw at this bug. And you can see in 1999 this is the pattern of resistance, mostly under about 10 percent across the United States. Now watch what happens when we play the video.
So I don't know where you live, but wherever it is, it certainly is a lot worse now than it was in 1999, and that is the problem of antibiotic resistance. It's a global issue affecting both rich and poor countries, and at the heart of it, you might say, well, isn't this really just a medical issue? If we taught doctors how not to use antibiotics as much, if we taught patients how not to demand antibiotics, perhaps this really wouldn't be an issue, and maybe the pharmaceutical companies should be working harder to develop more antibiotics. Now, it turns out that there's something fundamental about antibiotics which makes it different from other drugs, which is that if I misuse antibiotics or I use antibiotics, not only am I affected but others are affected as well, in the same way as if I choose to drive to work or take a plane to go somewhere, that the costs I impose on others through global climate change go everywhere, and I don't necessarily take these costs into consideration. This is what economists might call a problem of the commons, and the problem of the commons is exactly what we face in the case of antibiotics as well: that we don't consider — and we, including individuals, patients, hospitals, entire health systems — do not consider the costs that they impose on others by the way antibiotics are actually used.
Now, that's a problem that's similar to another area that we all know about, which is of fuel use and energy, and of course energy use both depletes energy as well as leads to local pollution and climate change. And typically, in the case of energy, there are two ways in which you can deal with the problem. One is, we can make better use of the oil that we have, and that's analogous to making better use of existing antibiotics, and we can do this in a number of ways that we'll talk about in a second, but the other option is the "drill, baby, drill" option, which in the case of antibiotics is to go find new antibiotics.
Now, these are not separate. They're related, because if we invest heavily in new oil wells, we reduce the incentives for conservation of oil in the same way that's going to happen for antibiotics. The reverse is also going to happen, which is that if we use our antibiotics appropriately, we don't necessarily have to make the investments in new drug development.
And if you thought that these two were entirely, fully balanced between these two options, you might consider the fact that this is really a game that we're playing. The game is really one of coevolution, and coevolution is, in this particular picture, between cheetahs and gazelles. Cheetahs have evolved to run faster, because if they didn't run faster, they wouldn't get any lunch. Gazelles have evolved to run faster because if they don't run faster, they would be lunch. Now, this is the game we're playing against the bacteria, except we're not the cheetahs, we're the gazelles, and the bacteria would, just in the course of this little talk, would have had kids and grandkids and figured out how to be resistant just by selection and trial and error, trying it over and over again. Whereas how do we stay ahead of the bacteria? We have drug discovery processes, screening molecules, we have clinical trials, and then, when we think we have a drug, then we have the FDA regulatory process. And once we go through all of that, then we try to stay one step ahead of the bacteria.
Now, this is clearly not a game that can be sustained, or one that we can win by simply innovating to stay ahead. We've got to slow the pace of coevolution down, and there are ideas that we can borrow from energy that are helpful in thinking about how we might want to do this in the case of antibiotics as well. Now, if you think about how we deal with energy pricing, for instance, we consider emissions taxes, which means we're imposing the costs of pollution on people who actually use that energy. We might consider doing that for antibiotics as well, and perhaps that would make sure that antibiotics actually get used appropriately. There are clean energy subsidies, which are to switch to fuels which don't pollute as much or perhaps don't need fossil fuels. Now, the analogy here is, perhaps we need to move away from using antibiotics, and if you think about it, what are good substitutes for antibiotics? Well, turns out that anything that reduces the need for the antibiotic would really work, so that could include improving hospital infection control or vaccinating people, particularly against the seasonal influenza. And the seasonal flu is probably the biggest driver of antibiotic use, both in this country as well as in many other countries, and that could really help. A third option might include something like tradeable permits. And these seem like faraway scenarios, but if you consider the fact that we might not have antibiotics for many people who have infections, we might consider the fact that we might want to allocate who actually gets to use some of these antibiotics over others, and some of these might have to be on the basis of clinical need, but also on the basis of pricing. And certainly consumer education works. Very often, people overuse antibiotics or prescribe too much without necessarily knowing that they do so, and feedback mechanisms have been found to be useful, both on energy — When you tell someone that they're using a lot of energy during peak hour, they tend to cut back, and the same sort of example has been performed even in the case of antibiotics. A hospital in St. Louis basically would put up on a chart the names of surgeons in the ordering of how much antibiotics they'd used in the previous month, and this was purely an informational feedback, there was no shaming, but essentially that provided some information back to surgeons that maybe they could rethink how they were using antibiotics.
Now, there's a lot that can be done on the supply side as well. If you look at the price of penicillin, the cost per day is about 10 cents. It's a fairly cheap drug. If you take drugs that have been introduced since then — linezolid or daptomycin — those are significantly more expensive, so to a world that has been used to paying 10 cents a day for antibiotics, the idea of paying 180 dollars per day seems like a lot. But what is that really telling us? That price is telling us that we should no longer take cheap, effective antibiotics as a given into the foreseeable future, and that price is a signal to us that perhaps we need to be paying much more attention to conservation. That price is also a signal that maybe we need to start looking at other technologies, in the same way that gasoline prices are a signal and an impetus, to, say, the development of electric cars. Prices are important signals and we need to pay attention, but we also need to consider the fact that although these high prices seem unusual for antibiotics, they're nothing compared to the price per day of some cancer drugs, which might save a patient's life only for a few months or perhaps a year, whereas antibiotics would potentially save a patient's life forever. So this is going to involve a whole new paradigm shift, and it's also a scary shift because in many parts of this country, in many parts of the world, the idea of paying 200 dollars for a day of antibiotic treatment is simply unimaginable. So we need to think about that.
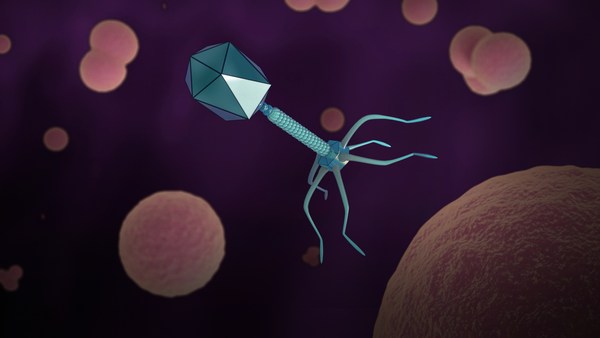
Now, there are backstop options, which is other alternative technologies that people are working on. It includes bacteriophages, probiotics, quorum sensing, synbiotics.
Now, all of these are useful avenues to pursue, and they will become even more lucrative when the price of new antibiotics starts going higher, and we've seen that the market does actually respond, and the government is now considering ways of subsidizing new antibiotics and development. But there are challenges here. We don't want to just throw money at a problem. What we want to be able to do is invest in new antibiotics in ways that actually encourage appropriate use and sales of those antibiotics, and that really is the challenge here.
Now, going back to these technologies, you all remember the line from that famous dinosaur film, "Nature will find a way." So it's not as if these are permanent solutions. We really have to remember that, whatever the technology might be, that nature will find some way to work around it.
You might think, well, this is just a problem just with antibiotics and with bacteria, but it turns out that we have the exact same identical problem in many other fields as well, with multidrug-resistant tuberculosis, which is a serious problem in India and South Africa. Thousands of patients are dying because the second-line drugs are so expensive, and in some instances, even those don't work and you have XDR TB. Viruses are becoming resistant. Agricultural pests. Malaria parasites. Right now, much of the world depends on one drug, artemisinin drugs, essentially to treat malaria. Resistance to artemisinin has already emerged, and if this were to become widespread, that puts at risk the single drug that we have to treat malaria around the world in a way that's currently safe and efficacious. Mosquitos develop resistance. If you have kids, you probably know about head lice, and if you're from New York City, I understand that the specialty there is bedbugs. So those are also resistant. And we have to bring an example from across the pond. Turns out that rats are also resistant to poisons.
Now, what's common to all of these things is the idea that we've had these technologies to control nature only for the last 70, 80 or 100 years and essentially in a blink, we have squandered our ability to control, because we have not recognized that natural selection and evolution was going to find a way to get back, and we need to completely rethink how we're going to use measures to control biological organisms, and rethink how we incentivize the development, introduction, in the case of antibiotics prescription, and use of these valuable resources. And we really now need to start thinking about them as natural resources. And so we stand at a crossroads. An option is to go through that rethinking and carefully consider incentives to change how we do business. The alternative is a world in which even a blade of grass is a potentially lethal weapon.
Thank you.
(Applause)