While regaling you with daring stories from her youth, it might be hard to believe your grandmother used to be a trapeze artist. However, the bad backs, elbow pain, and creaky knees so common in older people is more than just “old age." In fact, the source of this stiffness plagues many young people as well. The culprit is arthritis: a condition that causes inflammation and pain in the joints of over 90 million people in the U.S. alone. But are stiff, creaky joints really inevitable? What makes arthritis so pervasive, and why haven’t we found a cure for this widespread condition?
The first hurdle is that arthritis is actually a spectrum of over 100 different arthritic conditions. All these conditions share symptoms of joint pain and inflammation, but the origin and severity of those symptoms vary widely.
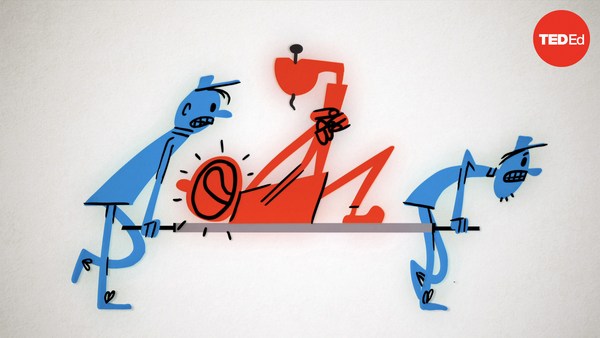
Even the most common type, osteoarthritis, is trickier to prevent than one might think. It’s a general misconception that arthritis is confined to old age. The origins of osteoarthritis can often be traced to a patient’s early life, from any seemingly ordinary joint injury. Following impact, immune cells rush in to help clean and repair the damaged site and begin pumping out enzymes, including matrix metalloproteinases and aggrecanases. These enzymes clear out the damaged tissue and contribute to inflammation. But while this rapid swelling helps protect the joint during recovery, inadequately healed tissue can cause these immune cells to overstay their welcome. The continuing flood of enzymes starts to degrade the cartilage, weakening the joint and leading to arthritis later on.
Not all forms of arthritis can simply be traced to an old sports injury. Take rheumatoid arthritis, which affects 1.3 million U.S. adults. This condition is actually an autoimmune disease in which autoantibodies target natively produced proteins, some of which are secreted by cartilage cells. We still don’t know what causes this behavior, but the result is that the body treats joint tissue like a foreign invader. Immune cells infiltrate the joint despite there being no tissue damage to repair. This response leads to chronic inflammation, which destroys bone and cartilage.
Yet another condition, spondyloarthritis, has similarities to both of the conditions we’ve covered. Patients experience continuous inflammation in the joints and at the sites where ligaments and tendons attach to bones, even without any initial injury. This leads to the flood of enzymes and degradation seen in osteoarthritis, but is driven by different inflammatory proteins called cytokines. As the enzymes eat away at cartilage, the body attempts to stabilize smaller joints by fusing them together. This process sometimes leads to outgrowths called bone spurs, which also cause intense stiffness and joint pain.
With so many factors causing arthritis, our current treatments are tailored to tackle specific symptoms rather than underlying causes. These range from promising MACI techniques, which harvest cells from small pieces of cartilage to grow replacement tissue. To a technique called microfracture, where surgeons create small holes in the bone, allowing bone marrow stem cells to leak out and form new cartilage. As a last resort, people with withered cartilage can even undergo full joint replacements.
But outside these drastic measures, the underlying drivers of autoimmune arthritis still present a unique treatment challenge. Scientists are making progress with therapies that block TNF-alpha, one of the primary proteins causing inflammation in rheumatoid arthritis. But even this approach only treats the symptoms of the condition, not the cause.
In the meantime, some of our best defenses against arthritis are lifestyle choices: maintaining a healthy weight to take pressure off joints, low-impact exercises like yoga or cycling, and avoiding smoking. These arthritis-fighting behaviors can help us lead longer lives as we continue to research cures and treatments for the huge diversity of arthritic conditions.